I've been diagnosed with lumbar spinal stenosis. What happens to people like me who get this condition?
Spinal stenosis describes a clinical syndrome of buttock or leg pain. These symptoms may occur with or without back pain. It is a condition in which the nerves in the spinal canal are closed in, or compressed.
The spinal canal is the hollow tube formed by the bones of the spinal column. Anything that causes this bony tube to shrink can squeeze the nerves inside. As a result of many years of wear and tear on the parts of the spine, bone spurs form, discs thin out, and spinal ligaments start to thicken. The result of any of these changes (and especially when combined together) is to cause pressure against the spinal nerves exiting the spinal canal.
This helps explain why lumbar spinal stenosis (stenosis of the low back) is a common cause of back problems in adults over 55 years old. But your question is what will happen now? You are asking about what physicians refer to as the natural history of a problem -- what happens over time.
The natural history isn't the same for everyone. There can be a variety of end-results. The symptoms can often be managed but the actual underlying changes in the spine don't go away. In some cases, things can get worse as pressure on the nerve tissue causes disabling pain and decreased quality of life. But that's the potential down-side. Let's look at the positive side of things.
We know from studies that treatment can be very effective in reducing symptoms and improving function. The first step to managing this condition is usually conservative (nonoperative) care. Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) are used to control pain and swelling.
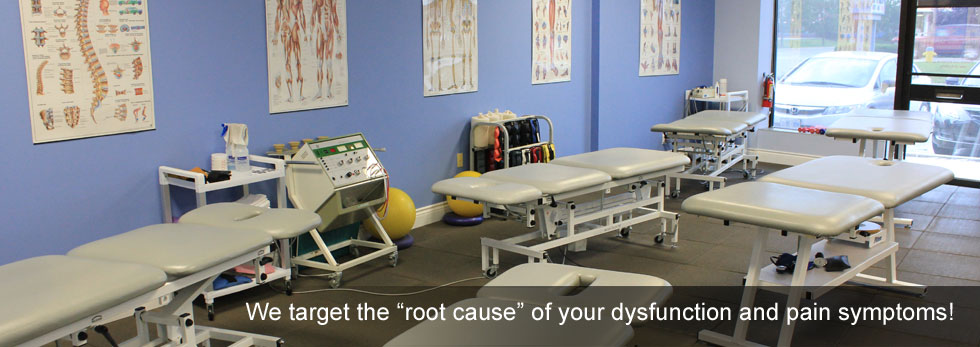
NSAIDs combined with physiotherapy may be all that some patients need. The physiotherapist addresses posture, strength (especially core strength), and modification of activities. The therapist can teach patients positions and exercises to ease the symptoms. The therapist may use lumbar traction to gently stretch and lengthen the low back, taking pressure off the spinal nerves.
Some patients are given an epidural steroid injection (ESI). The spinal cord is covered by a material called dura. The space between the dura and the spinal column is called the epidural space. It is thought that injecting steroid medication into this space fights inflammation around the nerves, the discs, and the facet joints. This can reduce swelling and give the nerves more room inside the spinal canal.
When conservative care doesn't work, then surgery may be advised. In fact, the results of the recent studies supports the use of surgery in such cases. When there is pain that doesn't go away with nonoperative care, decreased quality of life, or loss of function, surgery may be the only answer.
Studies and research investigation into the natural history of lumbar spinal stenosis are ongoing. Scientists hope to find ways to prevent this condition, limit the effects of stenosis, and treat it as effectively as possible when it does occur. Right now there are no known "cures" but management as described can be very effective.
Reference: Paul S. Issack, MD, PhD, et al. Degenerative Lumbar Spinal Stenosis: Evaluation and Management. In Journal of the American Academy of Orthopaedic Surgeons. August 2012. Vol. 20. No. 8. Pp. 527-535.