Introduction
Welcome to Sport And Spine Physiotherapy’s guide to gout.
 Gout is a disease that involves the build up of uric acid in the body. About 95 percent of gout patients are men. Most men are over 50 when gout first appears. When it does occur in women, they generally don't develop it until after menopause. In some rare cases gout develops at a young age.
Gout is a disease that involves the build up of uric acid in the body. About 95 percent of gout patients are men. Most men are over 50 when gout first appears. When it does occur in women, they generally don't develop it until after menopause. In some rare cases gout develops at a young age.
This guide will help you understand:
- how gout develops
- which parts of the body are affected by gout
- what can be done for the condition
- what Sport And Spine Physiotherapy’s approach to rehabilitation is
Anatomy
What is gout?
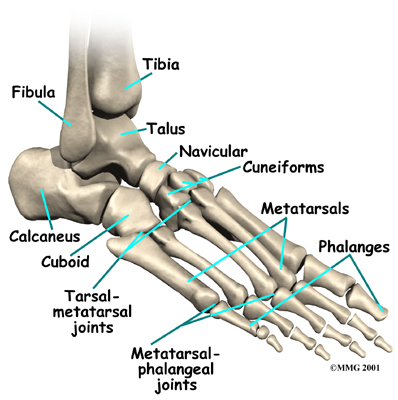
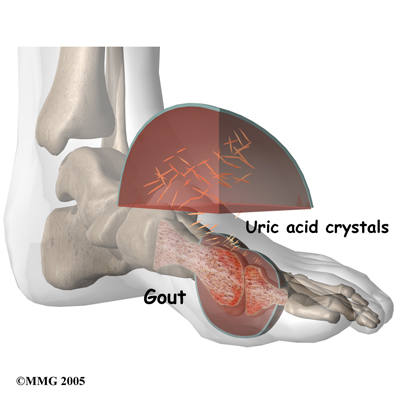
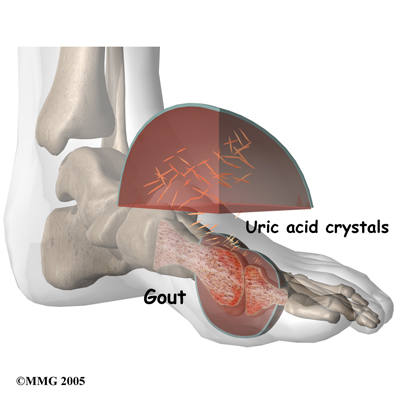
Synovial fluid is the fluid that the body produces to lubricate the joints. In gout, excess uric acid causes needle-shaped crystals to form in the synovial fluid. Uric acid is a normal chemical in the blood that comes from the breakdown of other chemicals in the body tissues. Everyone has some uric acid in his or her blood. As your immune system tries to get rid of the crystals in the synovial fluid, inflammation develops. For the person with too much uric acid, this inflammation can cause painful arthritis, sometimes called gouty arthritis. Gout was the first disease in which researchers recognized that crystals in the synovial fluid could be the cause of joint pain.
The first attack of gouty arthritis usually happens in just one joint. Half of the time, gout affects the metatarsophalangeal (MTP) joint at the base of the big toe. Eventually, 90 percent of people with gout will have pain in the MTP joint. Other joints that are commonly affected include the mid-foot, ankle, heel, and knee joints. Less commonly gout affects the fingers, wrists, and elbows.
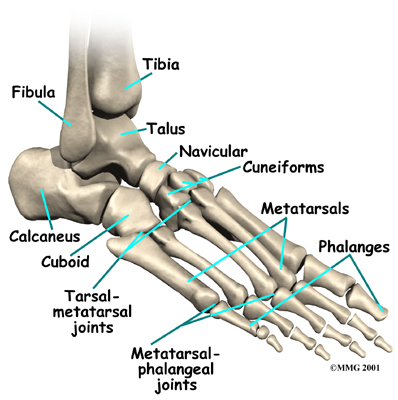
Over time, patients with gout can develop tophi, or lumps that grow around crystal deposits in joints or near pressure points. Tophi most often occur in the fingers, wrists, ears, knees, elbows, forearms, and heels. Tophi can also grow in the kidneys, heart, and eyes.
Symptoms
What does gout feel like?
Gout causes attacks of very painful joint inflammation. This pain is often described as a burning pain. Early gout attacks usually affect only one joint. As mentioned above, this joint is most commonly the MTP joint at the base of your big toe. The affected joint becomes swollen, warm, and red within eight to 12 hours. Most of the time the attacks occur at night and last 3-10 days. Patients indicate that the pain is so bad that the joint can't stand the slightest touch. Even the weight of a bed sheet causes excruciating pain. Walking and standing are almost impossible if the legs or feet are affected. Many patients have flu-like symptoms, including fever and chills. The pain may go away on its own over a few hours, or it may take a few weeks.
Gouty arthritis attacks come and go. There may be months between attacks. Over time the attacks generally occur more often, last longer, and involve more joints. Eventually the pain doesn't ever completely go away; the joints stay swollen and tender even between flare-ups, and the flare-ups start to happen every few weeks. As mentioned above, some patients eventually develop tophi on joints or pressure points as well as kidney stones.
Diagnosis
How do health care professionals identify the condition?
Early diagnosis of gout is important because crystals within the joint can lead to joint damage and this can occur without you knowing it. Patients with arthritic episodes that come and go may not seek medical help. Some patients are medically evaluated but complete testing is not done and they are misdiagnosed with rheumatoid arthritis. Either of these situations will delay treatment and increase the risk of erosive damage to the joint.
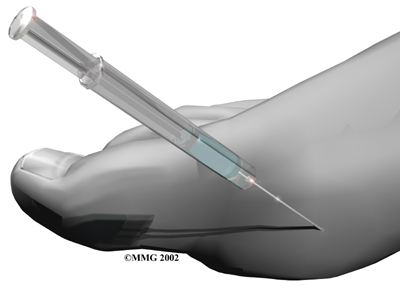
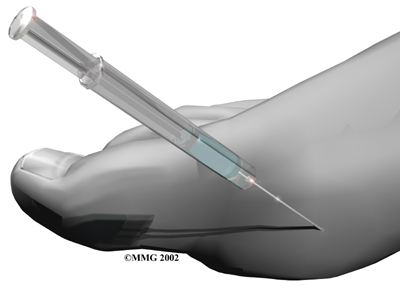
The diagnosis begins with a history of your symptoms and a physical exam. Your health care professional will want to know when the pain started, what aggravates or eases it, and if any other joints in your body are involved. They may also ask you about your diet, alcohol consumption, or whether or not you have a family history of gout or any other related medical conditions. The synovial fluid from the affected joint will need to be examined in order to identify the needle-like crystals that are part of gout. This is the most important part of the diagnosis. To get a sample of the synovial fluid, a doctor performs an arthrocentesis. During this procedure a long, thin needle is inserted into the affected joint and a small amount of synovial fluid is aspirated (removed.) The fluid is sent to a laboratory where it is viewed under a special polarized light microscope to determine if uric acid crystals are present.
If there are uric acid crystals present in the sampled synovial fluid, then you have gout. Unfortunately only 80 per cent of tests are positive when a person really has gout, so this test is not completely accurate. In some cases (such as in the midfoot), it isn't easy to aspirate fluid. Without the use of fluoroscopy (a special X-ray imaging) or ultrasound to guide the needle, aspiration isn't done. In these situations, the diagnosis is made without joint aspiration on the basis of the patient’s history and when they respond favorably to therapy aimed at treating gout.
The diagnosis must rule out the presence of infection, which can be a hidden problem. Your doctor may also get a blood test to look at the levels of uric acid. It should be noted, however, that uric acid levels rise and fall depending on many complex factors in your body. It is possible to have a normal uric acid level while you are having severe gout pain so this is not always a reliable indication of the presence of gout.
Ultrasonography may be helpful in the diagnosis of gout because the crystals form into the shape of rosary beads inside the cartilage on the ends of the bones and this can be seen on the ultrasound pictures. Ultrasonography can also show a ‘double contour sign.’ This sign looks like a top covering or extra coating of the joint surface when crystals are deposited in the hyaline cartilage. Ultrasonography, however, although very useful, should not replace fluid removal and examination in the diagnosis of gout because ultrasound cannot confirm infection.
If you have tophi, your doctor may want to biopsy one of the lumps.
As part of diagnosing gout your doctor will need to rule out other forms of arthritis as possible causes of your symptoms. Gout can occur with other forms of arthritis, such as septic arthritis and other forms of rheumatoid arthritis so the presence of these diseases will need to be determined. There are also other diseases that can cause different kinds of crystals to form in the synovial fluid so further investigation into whether other diseases are present may also need to be completed.
X-rays don't show doctors much in the early stages of gout. Despite this x-rays may be done as they can help monitor the disease process and they may be needed to rule out other problems.
Treatment
What can be done for this condition?
Gout cannot be cured, but it can be very successfully treated. The main goal of treating gout is to reduce the amount of urate in your blood. Joint crystals will not dissolve or go away unless the serum urate concentration is below six mg/dL.
During the acute or early phase of a gout attack, doctors prescribe medicines called colchicine, certain nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids to decrease swelling and relieve pain. All of these drugs work quickly and are very effective. The sooner they are given after an attack starts, the faster the pain goes away. These drugs may be given by mouth, through an intravenous line into your bloodstream, or injected directly into the joint. There are some potential adverse side effects of these medications. It may take a bit of time to find the most effective drug with the least intolerable side effects for some patients. Most importantly, one should start drug treatment during the first few days of an attack to get the best results.
Your doctor may also decompress the affected joint. Aspiration of synovial fluid immediately decreases the pressure in the joint and the needle leaves a pathway or track that acts as a vent for continued drainage after the needle is removed.
Lifestyle changes can help you manage intermittent gout without using drugs every day. Your healthcare professional may ask you to do the following:
Change your diet. Diets that are lower in meat, shellfish, and some other foods can help decrease the amount of uric acid in your body. Avoiding fructose sweetened foods and beverages can do the same.
- Quit taking drugs such as diuretics, if possible.
- Lose weight.
- Quit drinking alcohol.
- Avoid activities that stress your joints.
- Drink plenty of fluids to help your kidneys work more efficiently.
If your gout is severe, prolonged, or chronic, you may need to take daily serum uric acid-lowering (SUA) medication to reduce your uric acid levels. Your doctor will put you on the lowest dose possible of medications such as uricosuric drugs or xanthine oxidase inhibitors. Doctors usually prescribe allopurinol (Zyloprim, a xanthine oxidase inhibitor) for patients who overproduce urates or have tophi, kidney disease, or kidney stones. Allopurinol is useful in preventing recurrence of gouty attacks. It blocks the production of uric acid and decreases the formation of purine. For patients who have difficulty getting rid of uric acid through the kidneys, medications to help the kidneys remove more uric acid from the blood may be prescribed as well. Probenecid is one of the commonly prescribed drugs that increase the removal of uric acid in the urine.
Another serum uric acid-lowering (SUA) medication that has been shown to reduce the risk of occurrence is Uloric (Febuxostat). It lowers uric acid slowly enough to avoid flaring up the gout. The kidney doesn’t process this drug, so it's possible that patients with kidney disease may be able to take it. The liver, however, metabolizes this drug so anyone with a liver problem or who abuses alcohol may not be able to take this drug.
As with all medications, you should report any side effects to your doctor right away. Watch for skin rashes, itching, fever, nausea, vomiting, diarrhea, or other new symptoms not present before taking the serum uric acid medications.
Sometimes patients experience a flare-up after taking urate-lowering agents. This reaction can come as a surprise, since you expect your pain and swelling to get better. Flares of this kind mean that old deposits of crystals stored in the tissues are being released rather than a sign that new crystals are forming. To combat this, don't stop taking your medication without first checking with your doctor. Getting rid of the old crystals can help protect the joint from further damage.
Doctors seldom treat hyperuricemia without symptoms of gout. However, if hyperuricemia is at least moderately bad over several years, it is more likely to lead to gout. In this case, a doctor may begin treatments to prevent gout. This is called prophylactic treatment.
A program to control uric acid levels and manage symptoms often includes daily colchicine and allopurinol or probenecid (usually both are not taken at the same time) along with dietary restrictions. Regular follow-up with your physician and blood tests to detect serum uric acid concentration that are above the six mg/dL target level are important in maintaining good control and preventing joint erosion.
So far, there are no drug treatments to prevent the formation and deposit of these crystals in the joints. Researchers continue to look for pharmacological and other biologic therapies that might prevent, if not cure, gout for those who suffer from symptomatic outbreaks. Rehabilitation treatment and advice from a physiotherapist at Sport And Spine Physiotherapy can be of benefit for gout.
Sport And Spine Physiotherapy provides services for physiotherapy in Sarnia.
Rehabilitation
In some cases of gout when the joint flares up, treatment with a physiotherapist at Sport And Spine Physiotherapy can be helpful in conjunction with medication. Your therapist may use modalities such as ice, ultrasound, or laser to calm your joint down. You can also apply ice or a cold compress at home to soothe a joint flare up with gout. In many cases, however, direct physiotherapy treatment to the joint is too painful during a flare-up so resting and elevating the joint is the recommended treatment during this time.
Often when a joint is in a flare-up of gout, walking on the joint can be extremely painful or nearly impossible. Your physiotherapist can advise you on when you should use a walking aid such as a cane/stick to assist your gait. Walking without the proper support or with a limp for even a short period of time due to the pain of gout can cause you to develop incorrect gait patterns and put excess strain on the other joints of your body, particularly those in the lower extremities. Your therapist will also ensure that once your gout flare-up subsides that you are walking well and that you haven’t developed any poor long-term walking habits.
Being that repeated flare-ups of gout can eventually damage the joints and change the way they move and function, it is important that you maintain good range of motion in the joints, as well as flexibility and strength of the muscles surrounding the joints. Your physiotherapist will assess the joints that are commonly affected by gout in your case, and will prescribe range of motion, stretching, and strengthening exercises to help maintain the maximum function of the joints. Proprioception exercises, which assist in maintaining the joint’s sense of position, will also be prescribed. All exercises should be done between flare-ups rather than during a flare-up. Exercising a joint inflamed by gout is generally too painful, and may be detrimental to the joint due to the uric acid crystals that can wear on the joint surface during extreme motions of the joint.
As mentioned above, a sedentary lifestyle without exercise, obesity, as well as hypertension are all risk factors for developing gout. For this reason, at Sport And Spine Physiotherapy we feel it is important for all patients with gout to take part in a cardiovascular exercise program in order to reduce these risk factors, which can assist in decreasing the number of flare-ups of gout that occur. Your therapist can advise you on an appropriate cardiovascular exercise for you to partake in and can devise a program of exercise for you to follow. Some clients will find that doing a cardiovascular exercise in the pool, along with their other stretching and strengthening exercises, is easier and less painful on their joints. As with the other exercises mentioned above, cardiovascular exercise are best done between bouts of gout rather than during a flare-up.
Another risk factor for gout, as mentioned above, is diet. Alcohol, a high carbohydrate diet or one full of rich meats or sugary drinks will affect your gout. Your therapist can refer you to a Nutritionist to discuss altering your diet in order to help manage your gout.
Treatment for gout is a matter of management rather than elimination of the problem. By working closely with your doctor, physiotherapist and other healthcare professionals you can successfully manage the disease with as little impact as possible on your everyday life and activities.
Portions of this document copyright MMG, LLC.
Sport And Spine Physiotherapy provides services for physiotherapy in Sarnia.














 Gout is a disease that involves the build up of uric acid in the body. About 95 percent of gout patients are men. Most men are over 50 when gout first appears. When it does occur in women, they generally don't develop it until after menopause. In some rare cases gout develops at a young age.
Gout is a disease that involves the build up of uric acid in the body. About 95 percent of gout patients are men. Most men are over 50 when gout first appears. When it does occur in women, they generally don't develop it until after menopause. In some rare cases gout develops at a young age.